THE STORY OF AN INSOMNIAC
People's sleep needs vary. However, there’s scientific evidence that adults need an average of 7.5 hours of sleep. One insomniac shares their experience with sleep research.
PRELUDE OR IN THE SAME CLUB WITH THATCHER AND MADONNA
I’ve always slept very little; and I’ve considered it a positive fact that I have more extra hours per day than others. Margaret Thatcher, Winston Churchill, and Madonna allegedly also slept only four hours during their peak times! However, I wouldn’t be able to accomplish even a fraction of what they did during my additional hours of awake time … Anyway, being awake seems cool to me, and I hoped that as I age, my need for sleep would decrease even more. Unfortunately, instead of four hours, I’ve been sleeping for more like five, and when there’s time and no stress, sometimes even six hours. Yet, I sometimes feel quite tired during the day. Recent scientific studies on sleep tend to unanimously confirm that adults need preferably 7-8 hours of sleep for all the subtle functions of our body to work as needed and for us to enjoy a high-quality and long life. So, the thought that maybe I should have my sleep examined gradually crept into my mind.
SLEEP STUDIES
My sleep was studied at the 4 Kliinik. It requires spending a night in a sleep center with about twenty sensors and wires attached to the body and head. Initially, sleep disorder and emotional well-being questionnaires need to be filled out. It’s like taking a hard look in the mirror – when I’ve honestly recorded data about stress, blood pressure, wine, and sports, it’s clear that there’s either too much or too little of almost everything, and it’s on the wrong end of the scale. A couple of hours before falling asleep should be spent without electronic devices, and I try to do that as well. The sensors recorded my falling asleep at 1:11 am, which due to pure inactivity and boredom obviously is too early.
Despite the sensors protruding from my nose, wires coiling like snakes around my legs, and the rain drumming on the roof, the night seemed surprisingly suitable and calm for sleeping. And so, I slept soundly for five and a half hours and woke up the next day feeling refreshed like a puppy.
WHY DON’T WE SLEEP WELL?
Next, I met the somnologist and psychiatrist Tuuliki Hion to discuss the causes of insomnia that could be relieved with treatment. My results would also be interpreted and explained.
Let’s start by discussing the most common cause of reduced sleep–stress. Once stress has caused insomnia, it can become a persistent problem, and the body learns the pattern, leading to wakefulness at bedtime. In the worst cases, insomnia can persist for years, even when stress seems to have disappeared.
High blood pressure, sweating, nasal congestion, and going to the toilet more than once at night can be signs of sleep apnea, which is also a common cause of insomnia. Sleep apnea is a condition when the throat collapses, causing the body to wake up. If sleep apnea occurs during the REM sleep phase, in which we remember dreams better, and even though the cause is physical, it may feel that a nightmare is the reason for waking up.
Another significant sleep disturbing factor is the restless legs syndrome. The sleep-related part of restless legs is periodic limb movements, a frequently occurring sleep disorder that, like sleep apnea, can be alleviated with treatment.
DOCUMENTARY AND DIAGNOSIS
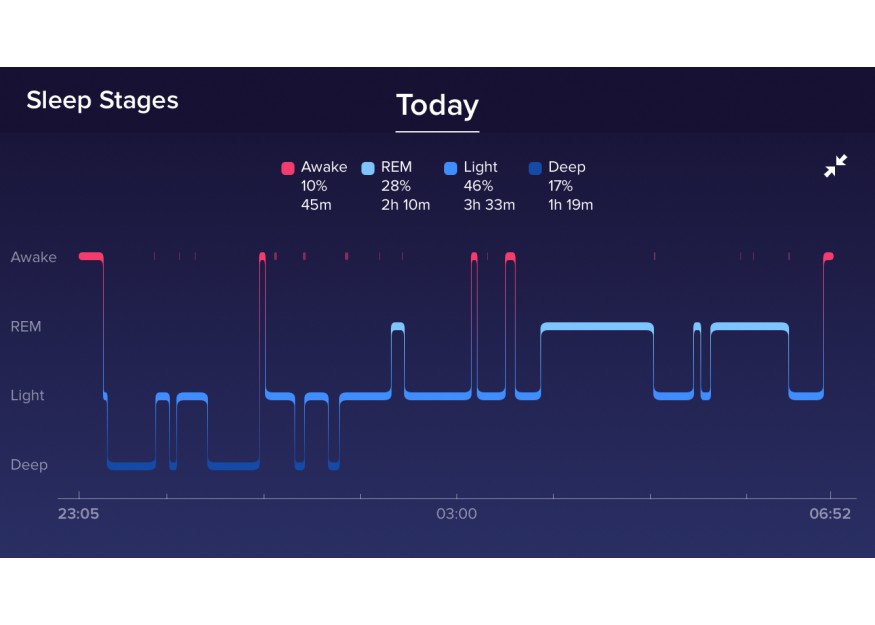
After reviewing the causes of insomnia, the doctor and I started watching my sleep video. I must admit that I’ve seen more exciting movies than the black-and-white footage of a person sleeping in a dark room. However, with Dr. Hion’s help and accompanying graphs, things became quite substantive and interesting. First, we analyzed my breathing. From this film, it became clear that the leading actress slept quietly without snoring. Still, the doctor knows that my breathing was disturbed – this was assessed based on changes in blood oxygen levels. The ideal oxygen saturation is 96%, but a 3% change is considered a breathing disorder. I had some plunges of 5-6%, indicating breathing pauses, which slightly affected both my pulse and blood pressure. However, as the nightly average was 95%, which is close to ideal, this shouldn’t be a significant problem in my case. Still, my number slightly exceeded the breathing disorder maximum regular index of 5.
Limb movements were also visible when my body was seeking an escape from the breathing disorder. But it quickly became clear that I also had an independent limb movement disorder because I moved after every few tens of seconds. According to the doctor, this could be one of the reasons I wake up at night and feel tired during the day, especially due to it raising both my pulse as well as blood pressure. The normal periodic limb movement index is up to 5, but mine is 23.
In summary, the doctor classified my sleep results as a combined problem, as both my breathing and limb movements need attention. However, since the latter is significantly above the norm, a one-month trial treatment was prescribed for me. The active ingredients of the medication are the same used for milder cases of restless legs and more severe cases of Parkinson’s disease. According to Dr. Hion, it usually takes a month to see if sleep quality and daytime well-being significantly improve. If not, it must be considered, whether another medication could help or if it’s better to address another symptom. Cognitive-behavioral therapy techniques for insomnia can also be used by anyone with sleep disorders, with or without breathing and movement disturbances. Good solutions and expert advice for combating insomnia are always available.
Egle Haidak